INFECTION PREVENTION AND CONTROL
Infection prevention and control (IPC) represents a critical
component of healthcare delivery aimed at minimizing the transmission of
infectious agents within healthcare settings. Academic discussion surrounding
IPC emphasizes a multifaceted approach encompassing various strategies to
mitigate the risk of healthcare associated infections (HAIs). Central to IPC is
the implementation of stringent protocols designed to optimize hand hygiene
practices among healthcare workers, as contaminated hands serve as significant
vectors for microbial transmission.
Additionally, the maintenance of a clean healthcare
environment through routine cleaning and disinfection protocols is necessary in
reducing pathogen reservoirs.
Furthermore, the prudent use of personal protective
equipment (PPE), including gloves, gowns, masks, and eye protection, serves to
safeguard both healthcare workers and patients from potential exposures.
In conclusion, effective infection prevention and control
measures can be established to support the highest standards of healthcare
quality and patient outcomes.
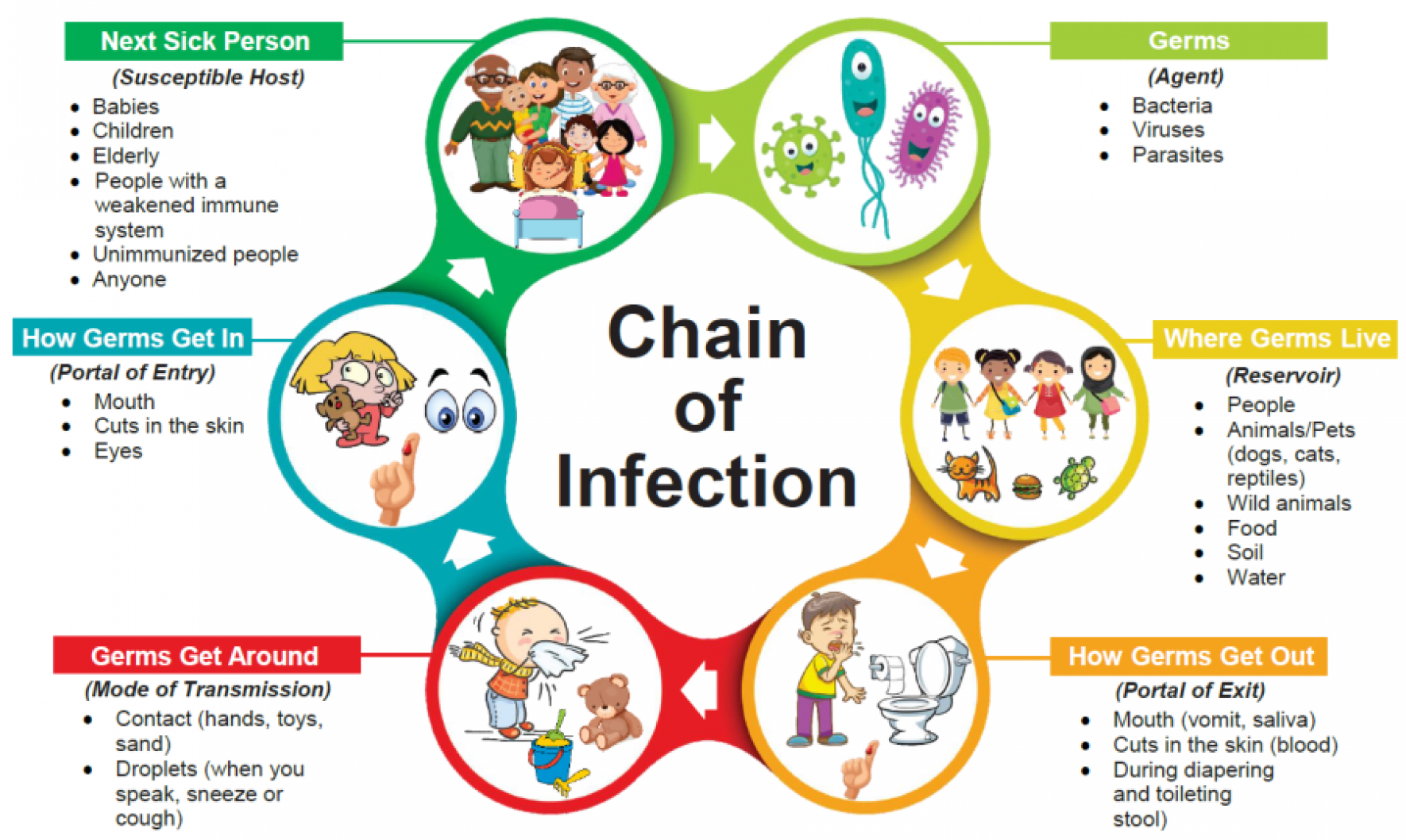
How infections spread?
Germs are a part of everyday life and are found in our air,
soil, water, and in and on our bodies. Some germs are helpful, others are
harmful. Many germs live in and on our bodies without causing harm and some
even help us to stay healthy. Infection spread follows a chain of events known
as the chain of infection, which consists of six interconnected links:
1.
Infectious Agent: the chain
begins with a pathogen, such as bacteria, viruses, fungi, or parasites, capable
of causing disease. Pathogens vary in their modes of transmission and
virulence.
2.
Reservoir/Source:
environment where a pathogen can live and multiplies. This can include humans,
animals, insects, environmental surfaces, or contaminated food and water.
3.
Portal of Exit: how the
pathogen exits or leaves reservoir, which can be bodily fluids (e.g.
respiratory droplets, blood, saliva, feces), skin lesions, or secretions.
4.
Modes of Transmission:
pathogens are transmitted from the reservoir to a susceptible host through
various modes, including direct contact (physical touch), indirect contact
(contaminated objects or surfaces), droplet transmission (respiratory droplets
expelled during coughing or sneezing), airborne transmission (inhalation of
small particles), and vector born transmission (via arthropods such as
mosquitoes or ticks).
5.
Portal of Entry: opening
where the pathogen may enter, common portals of entry include mucous membranes
(e.g. respiratory, gastrointestinal, genitourinary tracts), breaks in the skin
(e.g. cuts, wounds), or invasive medical devices (e.g. catheters, ventilators).
6.
Susceptible Host: finally,
the chain of infection depends on the presence of a susceptible host who lacks
effective immunity to the infectious agent. Factors influencing host
susceptibility include age, underlying health conditions, immune system,
nutrition).
Understanding and interrupting any link in the chain of
infection is essential for preventing and controlling the spread of infectious
diseases. Effective infection prevention measures focus on breaking this chain
through Standard Precautions and Transmission-Based Precautions.